Osteoporosis is a debilitating condition characterized by weakened bones, making them fragile and more susceptible to fractures.
Blog
Osteoporosis Pathophysiology: A Comprehensive Overview
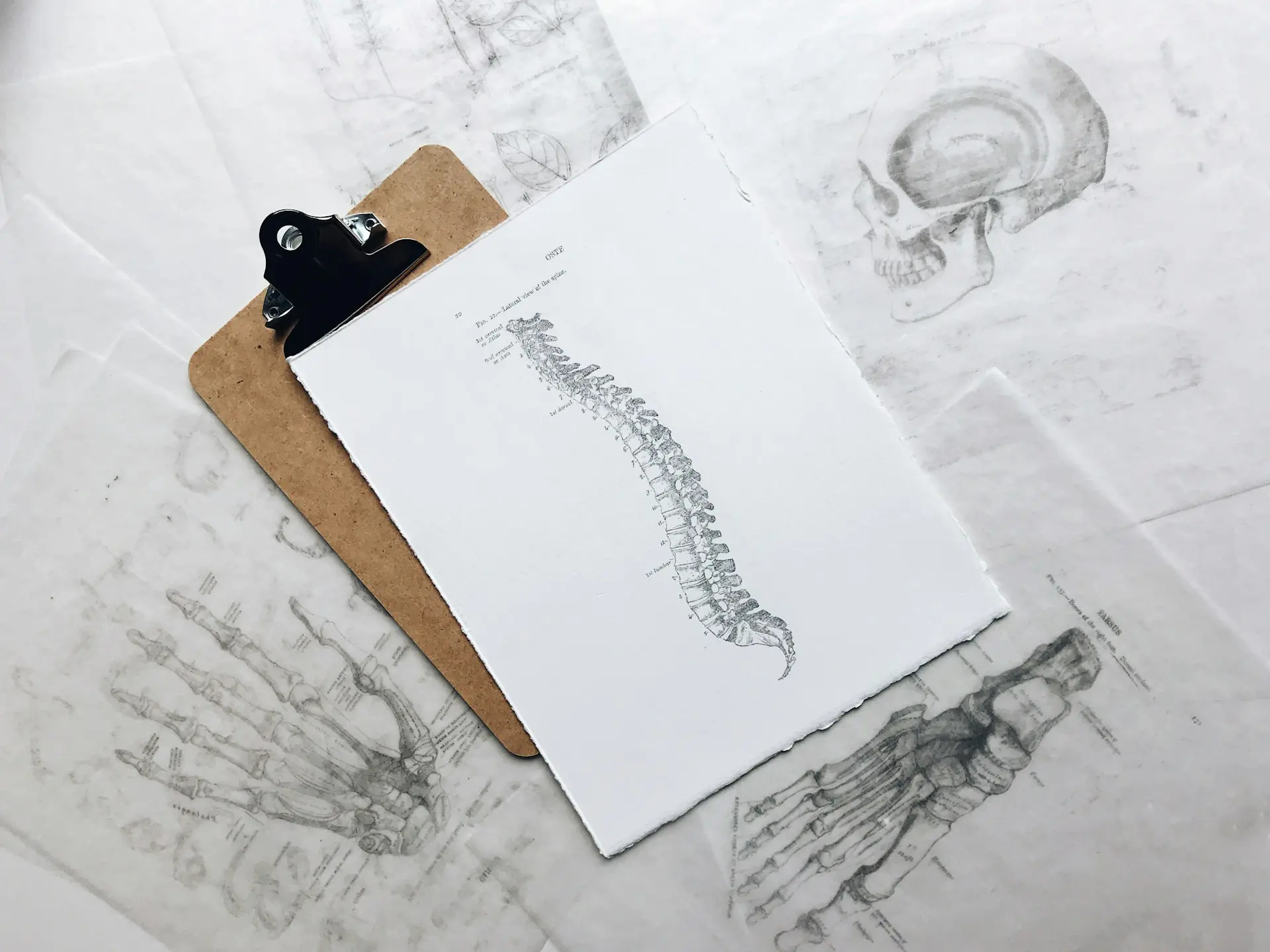
Osteoporosis is a debilitating condition characterized by weakened bones, making them fragile and more susceptible to fractures. Understanding the pathophysiology of osteoporosis is crucial for effective prevention and management strategies.
Bone is a dynamic tissue constantly undergoing remodeling, a process involving bone resorption by osteoclasts and formation by osteoblasts. In osteoporosis, there's an imbalance between bone resorption and formation, leading to a net loss of bone mass. This imbalance is primarily influenced by hormonal changes, aging, and lifestyle factors.
Hormones play a vital role in maintaining bone density and strength. Estrogen, in particular, plays a protective role in bone health by inhibiting bone resorption. However, during menopause, estrogen levels decline, resulting in accelerated bone loss in women. Similarly, low levels of testosterone in men can also contribute to bone loss and increase the risk of osteoporosis.
As individuals age, bone mass gradually declines due to decreased bone formation and increased bone resorption. This age-related bone loss is more pronounced in postmenopausal women and elderly individuals, predisposing them to osteoporosis-related fractures.
Genetics also play a significant role in determining an individual's susceptibility to osteoporosis. Certain genetic variations can influence bone density, structure, and turnover, thereby increasing the risk of developing osteoporosis later in life.
Several lifestyle factors can exacerbate bone loss and increase the risk of osteoporosis. These include sedentary lifestyle, poor nutrition, smoking, excessive alcohol consumption, and inadequate intake of calcium and vitamin D. Addressing these modifiable risk factors through lifestyle modifications is crucial for preventing osteoporosis.
In addition to age, hormonal changes, and lifestyle factors, certain medical conditions and medications can also contribute to secondary osteoporosis. Chronic conditions such as rheumatoid arthritis, hyperthyroidism, and gastrointestinal disorders can affect bone health, as can long-term use of corticosteroids and certain anticonvulsant medications.
Early detection of osteoporosis is essential for timely intervention and management. Diagnostic tools such as dual-energy X-ray absorptiometry (DXA) scans can assess bone mineral density and identify individuals at risk of fractures. Other tests, including biochemical markers of bone turnover, may also aid in evaluating bone health.
In conclusion, osteoporosis is a multifactorial condition influenced by various genetic, hormonal, age-related, and lifestyle factors. Understanding the pathophysiology of osteoporosis is crucial for implementing effective prevention and management strategies. By addressing modifiable risk factors, promoting bone health through adequate nutrition and exercise, and utilizing appropriate diagnostic tools, we can mitigate the impact of osteoporosis and improve the quality of life for affected individuals.
Bone is a dynamic tissue constantly undergoing remodeling, a process involving bone resorption by osteoclasts and formation by osteoblasts. In osteoporosis, there's an imbalance between bone resorption and formation, leading to a net loss of bone mass. This imbalance is primarily influenced by hormonal changes, aging, and lifestyle factors.
Hormones play a vital role in maintaining bone density and strength. Estrogen, in particular, plays a protective role in bone health by inhibiting bone resorption. However, during menopause, estrogen levels decline, resulting in accelerated bone loss in women. Similarly, low levels of testosterone in men can also contribute to bone loss and increase the risk of osteoporosis.
Genetics also play a significant role in determining an individual's susceptibility to osteoporosis. Certain genetic variations can influence bone density, structure, and turnover, thereby increasing the risk of developing osteoporosis later in life.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.