The pathogenesis of pneumonia involves the invasion of lung tissue by infectious agents, leading to inflammation and impaired gas exchange.
Blog
Pathogenesis of Pneumonia: Mechanisms and Implications
The pathogenesis of pneumonia involves the invasion of lung tissue by infectious agents, leading to inflammation and impaired gas exchange. Understanding the mechanisms of pneumonia is crucial for developing effective treatments and preventive strategies. Pneumonia is a significant cause of morbidity and mortality worldwide, affecting individuals of all ages.
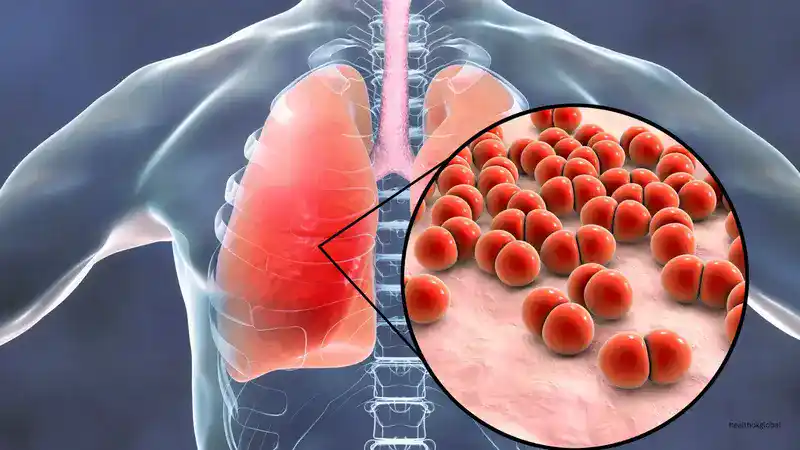
Pneumonia is an inflammatory condition of the lungs primarily caused by bacterial, viral, or fungal infections. It affects the alveoli, leading to the accumulation of fluid and impaired oxygen exchange. Pneumonia can range from mild to severe, and it is particularly dangerous for young children, the elderly, and individuals with compromised immune systems.
Pneumonia can be caused by a variety of pathogens, including bacteria (e.g., Streptococcus pneumoniae), viruses (e.g., influenza), and fungi (e.g., Pneumocystis jirovecii). The specific pathogen responsible for pneumonia can influence the severity and course of the disease. Bacterial pneumonia is often more severe and requires prompt antibiotic treatment.
The respiratory system has several defense mechanisms to protect against infections, including the mucociliary escalator, alveolar macrophages, and immune responses. When these defenses are compromised, pathogens can invade the lungs and cause pneumonia. Factors such as smoking, chronic lung diseases, and immunosuppression can weaken these defenses.
The pathophysiology of pneumonia involves the following steps: pathogen invasion, immune response, inflammation, and impaired gas exchange. The inflammatory response leads to the accumulation of fluid and immune cells in the alveoli, which impairs oxygen exchange and causes symptoms such as cough, fever, and difficulty breathing.
The clinical presentation of pneumonia varies depending on the causative pathogen, host factors, and severity of the infection. Common symptoms include cough, fever, chest pain, shortness of breath, and fatigue. In severe cases, patients may experience respiratory distress and require hospitalization. Early recognition and treatment are crucial for preventing complications.
Diagnosing pneumonia involves a combination of clinical evaluation, imaging studies, and laboratory tests. Chest X-rays and CT scans can reveal characteristic patterns of lung inflammation, while sputum cultures and blood tests help identify the causative pathogen. Timely and accurate diagnosis is essential for effective management.
The treatment of pneumonia depends on the causative pathogen and the patient's clinical condition. Bacterial pneumonia is typically treated with antibiotics, while antiviral or antifungal medications are used for viral and fungal pneumonia, respectively. Supportive care, including oxygen therapy and hydration, is also important for managing symptoms.
Complications of pneumonia can include respiratory failure, sepsis, lung abscesses, and pleural effusion. Early diagnosis and appropriate treatment are crucial to prevent these complications and improve patient outcomes. Long-term follow-up may be necessary for patients with chronic respiratory issues.
Preventing pneumonia involves vaccination, good hygiene practices, and addressing risk factors such as smoking and chronic diseases. Vaccines, such as the pneumococcal and influenza vaccines, are effective in reducing the incidence of pneumonia caused by specific pathogens. Public health initiatives should focus on increasing vaccination coverage and promoting healthy lifestyles.
Public health initiatives play a vital role in reducing the burden of pneumonia. These include education campaigns to promote vaccination, improving access to healthcare services, and implementing strategies to reduce the spread of respiratory infections. Collaborative efforts between healthcare providers and public health organizations are essential for effective prevention and control.
Ongoing research aims to develop more effective vaccines and treatments for pneumonia. Advances in understanding the molecular mechanisms of pneumonia pathogenesis will contribute to the development of targeted therapies and improved public health strategies. Innovations in diagnostic tools and treatment protocols are essential for reducing pneumonia-related morbidity and mortality.
Understanding the pathogenesis of pneumonia is essential for developing effective strategies to prevent and treat this common lung infection. By exploring the mechanisms involved in pathogen invasion, immune response, and inflammation, we can better appreciate the complexities of pneumonia and work towards improved treatments and preventive measures. Continued research and public health efforts are crucial in reducing the burden of pneumonia and improving patient outcomes. A comprehensive approach that includes vaccination, early diagnosis, and effective treatment can significantly reduce the impact of pneumonia on global health.
Pneumonia is an inflammatory condition of the lungs primarily caused by bacterial, viral, or fungal infections. It affects the alveoli, leading to the accumulation of fluid and impaired oxygen exchange. Pneumonia can range from mild to severe, and it is particularly dangerous for young children, the elderly, and individuals with compromised immune systems.
Pneumonia can be caused by a variety of pathogens, including bacteria (e.g., Streptococcus pneumoniae), viruses (e.g., influenza), and fungi (e.g., Pneumocystis jirovecii). The specific pathogen responsible for pneumonia can influence the severity and course of the disease. Bacterial pneumonia is often more severe and requires prompt antibiotic treatment.
Ongoing research aims to develop more effective vaccines and treatments for pneumonia. Advances in understanding the molecular mechanisms of pneumonia pathogenesis will contribute to the development of targeted therapies and improved public health strategies. Innovations in diagnostic tools and treatment protocols are essential for reducing pneumonia-related morbidity and mortality.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.