Intestinal tuberculosis is a form of TB that affects the gastrointestinal tract, presenting with various symptoms and requiring specific diagnostic and treatment approaches.
Blog
Intestinal Tuberculosis: Symptoms, Diagnosis, and Treatment
Intestinal tuberculosis is a form of TB that affects the gastrointestinal tract, presenting with various symptoms and requiring specific diagnostic and treatment approaches. Understanding intestinal TB is crucial for effective management and improving patient outcomes. This blog delves into the complexities of intestinal TB, its symptoms, diagnosis, and treatment.
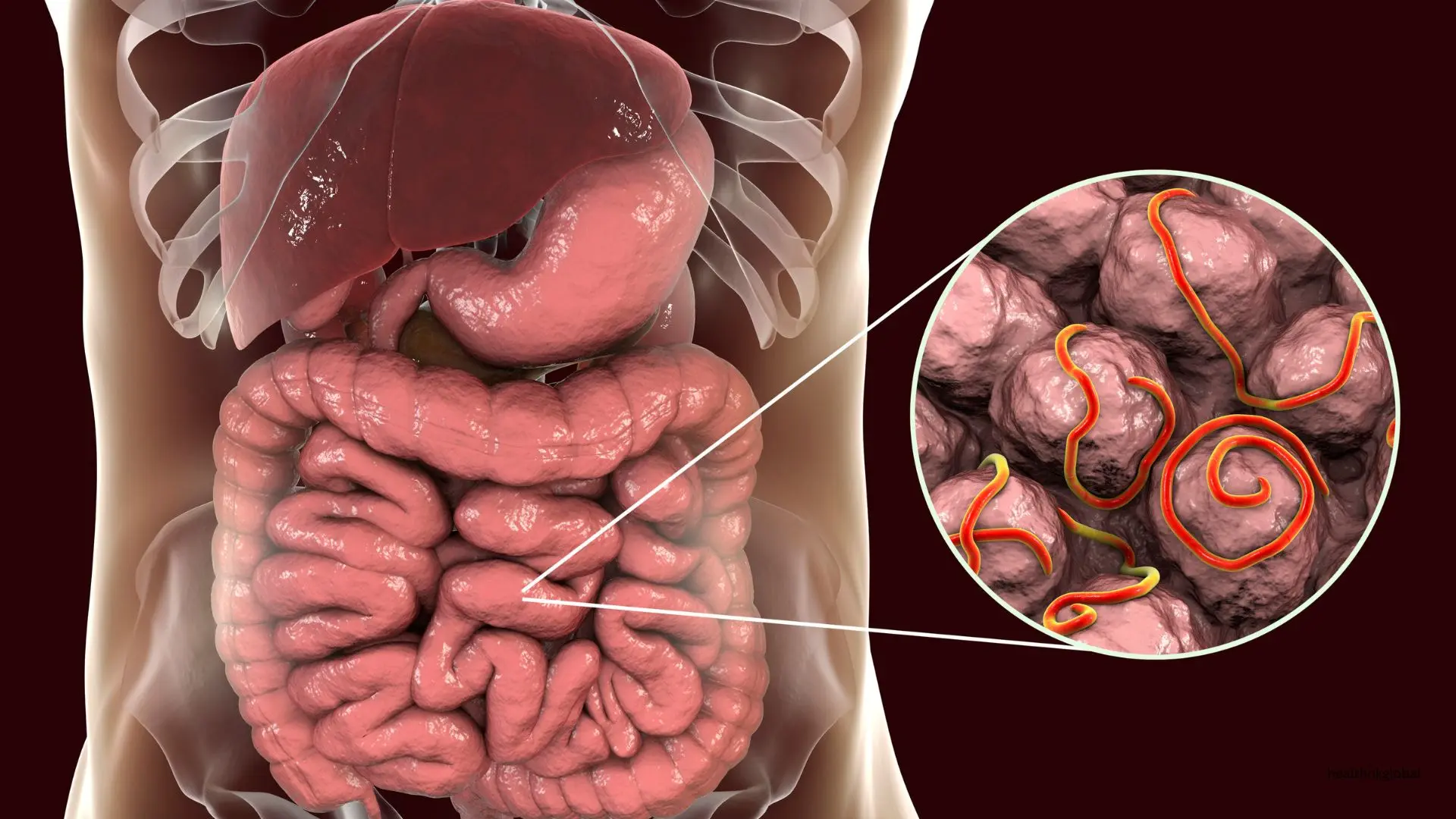
Intestinal tuberculosis, also known as abdominal TB, primarily affects the small intestine, but can also involve the stomach, large intestine, and peritoneum. It is caused by the Mycobacterium tuberculosis bacterium and is often associated with pulmonary TB. Intestinal TB can mimic other gastrointestinal conditions, making diagnosis challenging.
The symptoms of intestinal TB can be non-specific and vary depending on the site of infection. Common symptoms include abdominal pain, diarrhea, weight loss, fever, and a palpable abdominal mass. In some cases, patients may experience bowel obstruction or perforation. Chronic symptoms can lead to significant morbidity if not promptly treated.
Risk factors for developing intestinal TB include immunosuppression (e.g., HIV infection), malnutrition, and a history of pulmonary TB. Individuals living in areas with high TB prevalence are also at increased risk. Early identification and management of these risk factors are crucial for preventing the spread of TB.
Diagnosing intestinal TB involves a combination of clinical evaluation, radiographic imaging, and laboratory tests. Endoscopy with biopsy is often performed to obtain tissue samples for histopathological examination and culture. Imaging studies such as CT scans and ultrasounds can help identify characteristic features of intestinal TB.
Intestinal TB can mimic other gastrointestinal conditions, making differential diagnosis challenging. Conditions such as Crohn's disease, colorectal cancer, and other infectious diseases must be considered and ruled out during evaluation. Accurate diagnosis requires a multidisciplinary approach and collaboration between gastroenterologists and infectious disease specialists.
The treatment of intestinal TB involves a combination of anti-tubercular drugs administered over several months. The standard regimen includes isoniazid, rifampicin, ethambutol, and pyrazinamide. Surgical intervention may be required in cases of bowel obstruction, perforation, or abscess formation. Adherence to the treatment regimen is crucial for successful outcomes.
Complications of untreated or inadequately treated intestinal TB can be severe and include intestinal obstruction, perforation, abscess formation, and fistulae. Early diagnosis and appropriate treatment are crucial to prevent these complications. Long-term follow-up is essential to monitor for potential relapse and manage any chronic complications.
Preventing intestinal TB involves addressing the broader issue of TB control. This includes early detection and treatment of pulmonary TB, improving living conditions, and ensuring adequate nutrition. The BCG vaccine can provide some protection against TB, although its efficacy in preventing intestinal TB is limited.
Public health measures play a critical role in controlling the spread of tuberculosis. This includes education on TB transmission and prevention, improving access to healthcare services, and implementing strategies to reduce the social determinants of health that contribute to TB. Community engagement and awareness campaigns are essential components of these measures.
Research is ongoing to develop more effective diagnostic tools and treatment regimens for intestinal TB. Advances in molecular diagnostics and drug development hold promise for improving patient outcomes and reducing the global burden of TB. Collaborative efforts between researchers, healthcare providers, and policymakers are essential for achieving these goals.
Intestinal tuberculosis is a serious form of TB that affects the gastrointestinal tract and requires timely diagnosis and treatment. Understanding its symptoms, risk factors, and diagnostic methods is essential for effective management. By addressing the broader issue of TB control and improving public health measures, we can reduce the incidence of intestinal TB and improve patient outcomes. Ongoing research and global collaboration are vital to combating this infectious disease.
Intestinal tuberculosis, also known as abdominal TB, primarily affects the small intestine, but can also involve the stomach, large intestine, and peritoneum. It is caused by the Mycobacterium tuberculosis bacterium and is often associated with pulmonary TB. Intestinal TB can mimic other gastrointestinal conditions, making diagnosis challenging.
The symptoms of intestinal TB can be non-specific and vary depending on the site of infection. Common symptoms include abdominal pain, diarrhea, weight loss, fever, and a palpable abdominal mass. In some cases, patients may experience bowel obstruction or perforation. Chronic symptoms can lead to significant morbidity if not promptly treated.
Preventing intestinal TB involves addressing the broader issue of TB control. This includes early detection and treatment of pulmonary TB, improving living conditions, and ensuring adequate nutrition. The BCG vaccine can provide some protection against TB, although its efficacy in preventing intestinal TB is limited.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.