Diabetes is a chronic condition that requires comprehensive management to ensure a high quality of life.

Blog
Nursing Care Plan Guide for Diabetes: Symptoms, Treatment, and Management
Diabetes is a chronic condition characterized by high levels of glucose in the blood. It results from either insufficient insulin production by the pancreas or the body's inability to effectively use the insulin it produces. Diabetes can lead to serious health complications if not managed properly. A comprehensive nursing care plan for diabetes involves understanding the symptoms, providing effective treatment, and implementing management strategies to help patients maintain optimal health. This guide covers various aspects of diabetes care, from diagnosis to long-term management.
Diabetes can be classified into three main types: Type 1 diabetes, Type 2 diabetes, and gestational diabetes. Each type has distinct characteristics and requires different approaches to management.
Type 1 diabetes is characterized by sudden onset of symptoms such as excessive thirst, frequent urination, weight loss, fatigue, and blurred vision. It often occurs in children and young adults.
Diagnosis involves blood tests to measure blood glucose levels, HbA1c levels, and the presence of autoantibodies.
Type 2 diabetes develops gradually and is often associated with symptoms such as increased thirst, frequent urination, hunger, fatigue, and blurred vision. It is more common in adults but can also occur in children and adolescents.
Diagnosis is confirmed through blood tests, including fasting blood glucose, oral glucose tolerance test, and HbA1c levels.
Gestational diabetes is usually asymptomatic but can be detected through routine screening during pregnancy. It involves elevated blood glucose levels that develop during pregnancy.
Diagnosis is made through glucose tolerance tests conducted during pregnancy.
Accurate diagnosis is essential for developing an effective nursing care plan for diabetes. This involves a comprehensive evaluation by a healthcare provider.
The healthcare provider will review the patient's medical history, including any family history of diabetes, current symptoms, and lifestyle factors.
A detailed discussion of the patient's symptoms, including their onset, duration, and impact on daily life, is crucial for accurate diagnosis.
A physical exam may be conducted to assess for signs of diabetes complications, such as neuropathy, retinopathy, and skin changes.
Blood tests are performed to measure blood glucose levels, HbA1c, and other relevant parameters.
A fasting blood glucose level of 126 mg/dL or higher on two separate occasions indicates diabetes.
An HbA1c level of 6.5% or higher indicates diabetes.
A 2-hour blood glucose level of 200 mg/dL or higher during an OGTT indicates diabetes.
The treatment of diabetes involves a combination of lifestyle changes, medications, and regular monitoring. The goal is to maintain blood glucose levels within the target range and prevent complications.
A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is essential for managing diabetes. Monitoring carbohydrate intake and portion sizes helps maintain stable blood glucose levels.
Engaging in regular physical activity, such as walking, cycling, or swimming, helps improve insulin sensitivity and manage blood glucose levels.
Achieving and maintaining a healthy weight through diet and exercise can significantly improve blood glucose control.
Insulin therapy is essential for individuals with Type 1 diabetes and may be necessary for those with Type 2 diabetes who do not respond to oral medications. Various types of insulin, including rapid-acting, long-acting, and combination insulins, are used to manage blood glucose levels.
Oral medications, such as metformin, sulfonylureas, and DPP-4 inhibitors, help manage blood glucose levels in individuals with Type 2 diabetes.
These injectable medications help lower blood glucose levels and promote weight loss in individuals with Type 2 diabetes.
Regular self-monitoring of blood glucose levels using a glucometer helps patients track their blood glucose levels and adjust their treatment plan as needed.
CGM devices provide real-time blood glucose readings and trends, helping patients make informed decisions about their diabetes management.
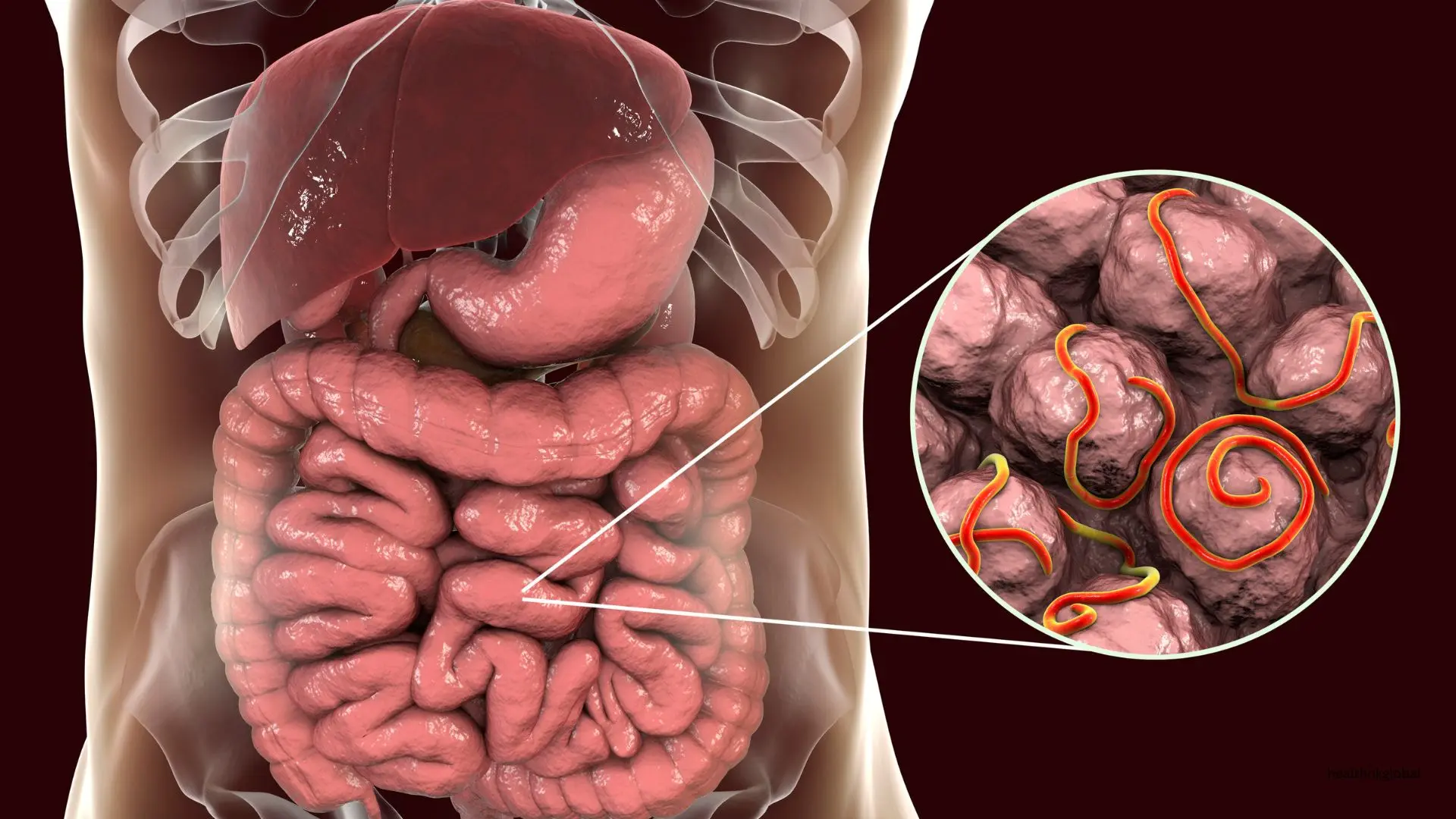
Regular foot care, pain management, and medications to improve nerve function are essential for managing diabetic neuropathy.
Regular eye exams, blood glucose control, and laser treatments can help prevent and manage diabetic retinopathy.
Controlling blood glucose and blood pressure, along with medications such as ACE inhibitors, can help manage diabetic nephropathy.
Nurses play a vital role in the management and education of patients with diabetes. Effective nursing care strategies include patient education, care coordination, and ongoing support.
Educating patients about the nature of diabetes, its complications, and the importance of blood glucose control is crucial for effective self-management.
Emphasizing the importance of taking prescribed medications as directed and educating patients about the potential side effects.
Providing guidance on healthy eating, physical activity, and weight management to help patients achieve optimal blood glucose control.
Collaborating with other healthcare professionals, such as dietitians, endocrinologists, and podiatrists, to provide comprehensive care for patients with diabetes.
Scheduling regular follow-up appointments to monitor the patient's progress, adjust the treatment plan, and address any concerns or complications.
Encouraging participation in diabetes support groups to provide emotional support and share experiences with others facing similar challenges.
Providing access to mental health resources, such as counseling and stress management techniques, to help patients cope with the emotional aspects of diabetes management.
A comprehensive nursing care plan for diabetes encompasses accurate diagnosis, effective treatment, and ongoing management. By addressing the underlying causes and providing targeted interventions, patients with diabetes can achieve significant improvements in their health and quality of life. Regular monitoring, lifestyle modifications, and patient education are essential components of a successful diabetes management strategy. Nurses play a crucial role in supporting patients throughout their diabetes journey, ensuring they receive the care and guidance needed to manage their condition effectively.
Diabetes can be classified into three main types: Type 1 diabetes, Type 2 diabetes, and gestational diabetes. Each type has distinct characteristics and requires different approaches to management.
Type 1 diabetes is characterized by sudden onset of symptoms such as excessive thirst, frequent urination, weight loss, fatigue, and blurred vision. It often occurs in children and young adults.
This section covers 3. Ongoing Support in detail.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.