Peptic ulcers are sores that develop on the lining of the stomach, small intestine, or esophagus, causing significant discomfort and potential complications.
Blog
Comprehensive Nursing Management of Peptic Ulcer
Peptic ulcers are sores that develop on the lining of the stomach, small intestine, or esophagus, causing significant discomfort and potential complications. Effective nursing management is crucial for promoting healing, preventing complications, and providing patient education. This blog explores the comprehensive nursing management of peptic ulcers, focusing on care strategies, patient education, and interventions to ensure optimal patient outcomes.
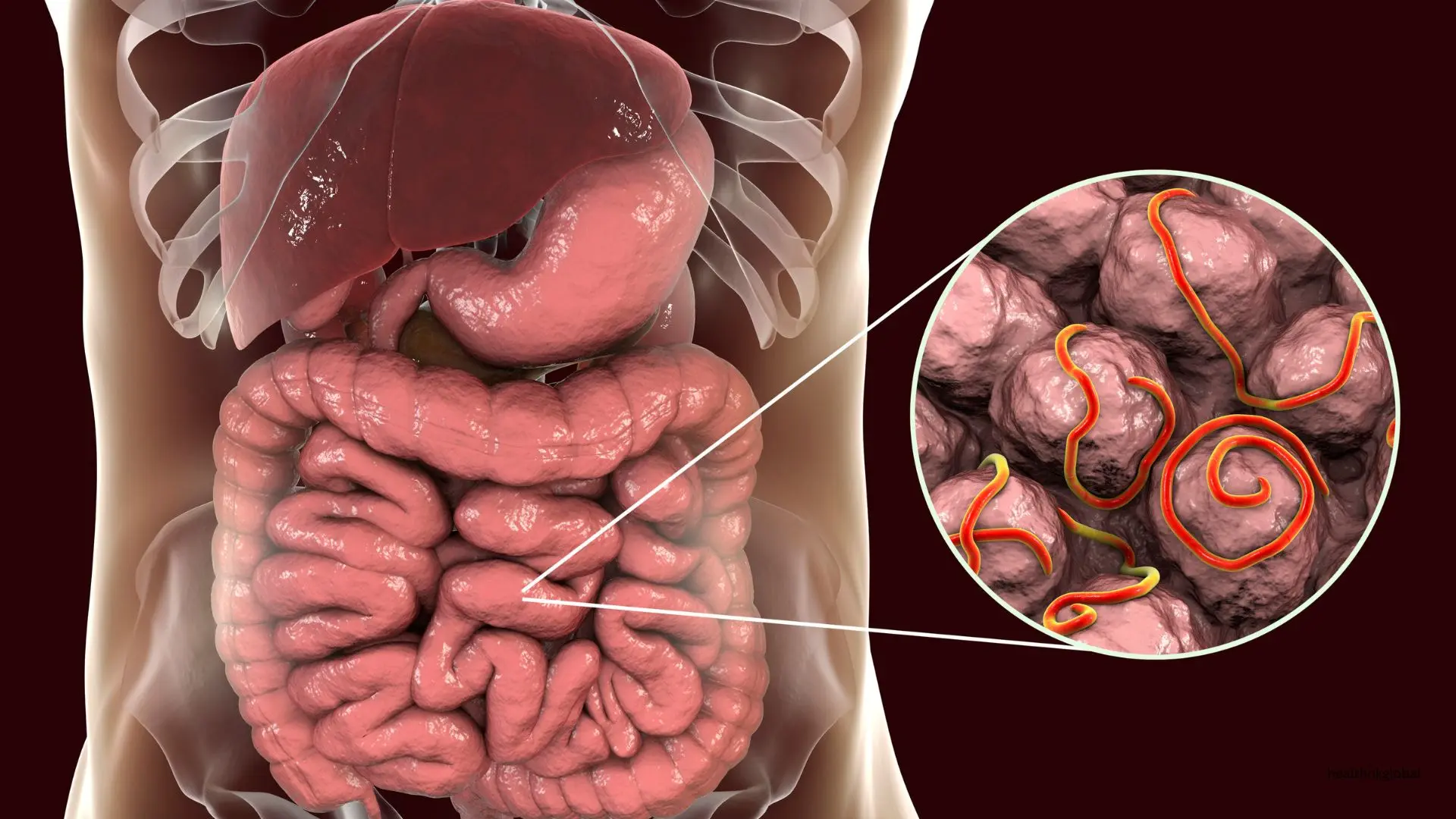
Peptic ulcers occur when the protective lining of the stomach or duodenum is damaged by stomach acid. This damage can be caused by infection with Helicobacter pylori (H. pylori), long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, smoking, and stress. Symptoms of peptic ulcers include abdominal pain, bloating, nausea, vomiting, and, in severe cases, bleeding.
The first step in nursing management is a thorough assessment and accurate diagnosis. This includes taking a detailed patient history, conducting a physical examination, and ordering diagnostic tests such as endoscopy, H. pylori testing, and imaging studies. Identifying the underlying cause of the ulcer is essential for developing an effective treatment plan.
Medication is a cornerstone of peptic ulcer treatment. Nurses play a vital role in administering medications and monitoring their effectiveness. Common medications used include:
PPIs reduce stomach acid production, promoting ulcer healing. Examples include omeprazole, esomeprazole, and pantoprazole.
These medications also reduce stomach acid. Examples include ranitidine and famotidine.
For H. pylori infection, a combination of antibiotics such as amoxicillin, clarithromycin, and metronidazole is prescribed.
Antacids neutralize stomach acid and provide quick relief from pain. Examples include aluminum hydroxide and magnesium hydroxide.
Educating patients about their condition, treatment, and lifestyle modifications is crucial for effective management. Key points to cover include:
Instruct patients on the importance of taking medications as prescribed and completing the full course of antibiotics if applicable.
Encourage patients to avoid foods and beverages that can irritate the stomach lining, such as spicy foods, caffeine, and alcohol.
Teach patients stress reduction techniques such as relaxation exercises, meditation, and yoga.
Provide resources and support for quitting smoking, as it can exacerbate ulcer symptoms and delay healing.
Advise patients to limit or avoid alcohol consumption to prevent further irritation of the stomach lining.
Regular monitoring and follow-up are essential components of nursing management. This includes assessing symptom improvement, monitoring for potential complications, and ensuring adherence to the treatment plan. Follow-up appointments should be scheduled to evaluate the effectiveness of treatment and make necessary adjustments.
Preventing complications is a key aspect of nursing care. Nurses should educate patients about the signs and symptoms of potential complications such as perforation, bleeding, and gastric obstruction. Prompt recognition and intervention are critical to prevent serious outcomes.
Providing nutritional support is vital for patients with peptic ulcers. A diet rich in fiber, fruits, and vegetables can promote healing and overall health. Nurses should work with dietitians to develop personalized meal plans that meet the patient's nutritional needs and preferences.
Encouraging lifestyle modifications can significantly improve patient outcomes. In addition to dietary changes, patients should be advised to maintain a healthy weight, engage in regular physical activity, and avoid the use of NSAIDs unless absolutely necessary.
Effective nursing management of peptic ulcers involves a comprehensive approach that includes assessment, medication management, patient education, monitoring, and lifestyle modifications. By providing holistic care and educating patients about their condition, nurses can help promote healing, prevent complications, and improve overall quality of life. Regular follow-up and collaboration with the healthcare team are essential to ensure the best outcomes for patients with peptic ulcers.
HealthOK Global provides expert insights on nutrition, meal planning, and healthy eating habits. Contact our FREE 24 x 7 Healthcare Helpline at +91-8047190955 for assistance.
Peptic ulcers occur when the protective lining of the stomach or duodenum is damaged by stomach acid. This damage can be caused by infection with Helicobacter pylori (H. pylori), long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, smoking, and stress. Symptoms of peptic ulcers include abdominal pain, bloating, nausea, vomiting, and, in severe cases, bleeding.
The first step in nursing management is a thorough assessment and accurate diagnosis. This includes taking a detailed patient history, conducting a physical examination, and ordering diagnostic tests such as endoscopy, H. pylori testing, and imaging studies. Identifying the underlying cause of the ulcer is essential for developing an effective treatment plan.
Encouraging lifestyle modifications can significantly improve patient outcomes. In addition to dietary changes, patients should be advised to maintain a healthy weight, engage in regular physical activity, and avoid the use of NSAIDs unless absolutely necessary.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.