The pathophysiology of tuberculosis involves complex interactions between the Mycobacterium tuberculosis bacterium and the host's immune system.
Blog
Pathophysiology of Tuberculosis: Mechanisms and Implications
The pathophysiology of tuberculosis involves complex interactions between the Mycobacterium tuberculosis bacterium and the host's immune system. Understanding these mechanisms is crucial for developing effective treatments and preventive strategies. Tuberculosis (TB) is a major global health issue, affecting millions of people worldwide. It is essential to understand the underlying mechanisms of this disease to combat its spread and improve treatment outcomes.
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also impact other parts of the body, including the kidneys, spine, and brain. TB is transmitted through airborne droplets when an infected person coughs or sneezes. Despite significant advancements in medicine, TB remains a leading cause of death worldwide, particularly in low- and middle-income countries.
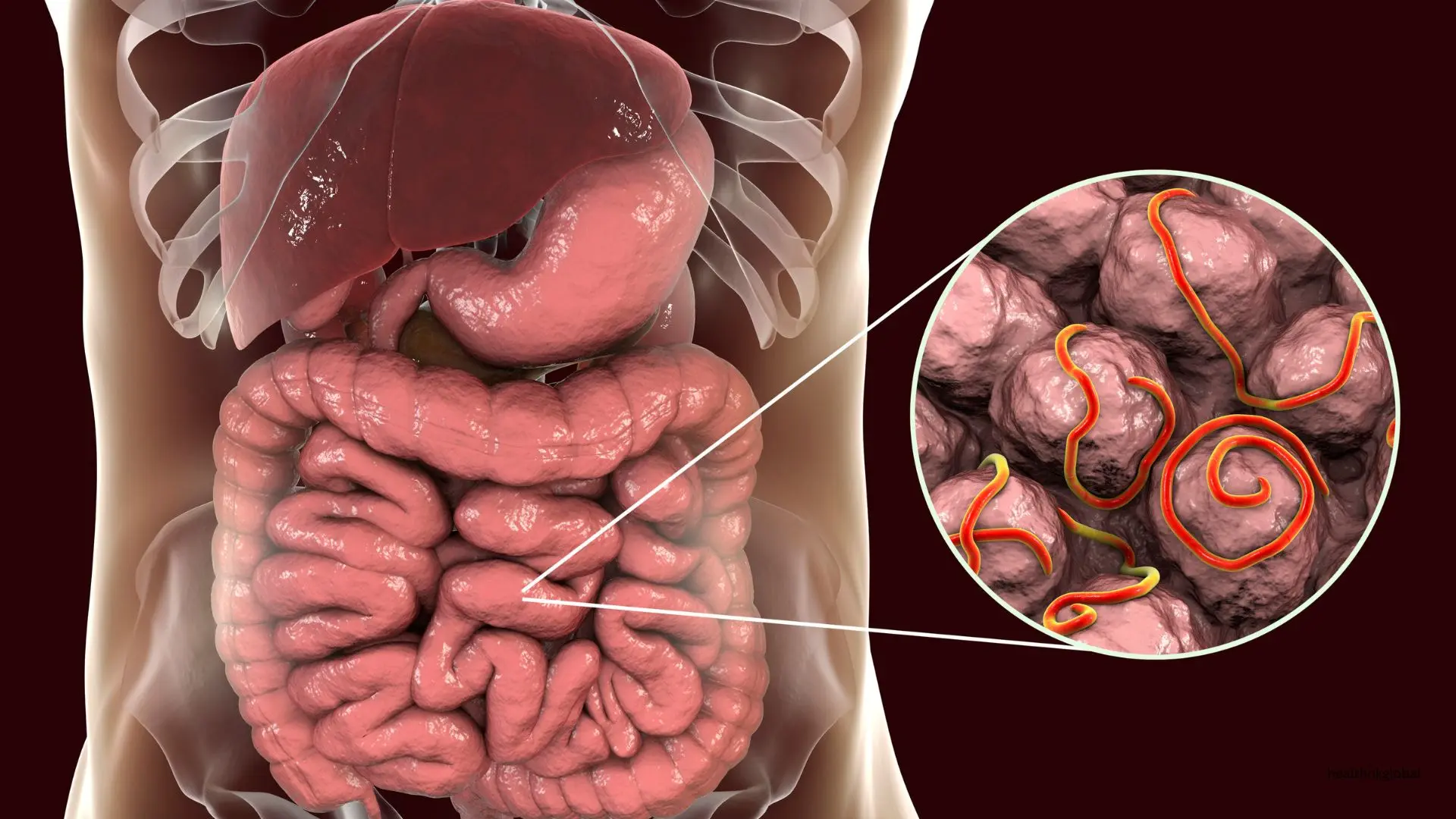
The pathogenesis of tuberculosis involves several stages, including initial infection, latent TB, and active TB. During initial infection, the bacterium enters the lungs and is engulfed by alveolar macrophages. However, Mycobacterium tuberculosis can evade the immune response, leading to the formation of granulomas, which contain the infection but do not eliminate it. This complex process involves multiple factors, including bacterial virulence and host immune responses.
The immune response to TB is complex and involves both innate and adaptive immunity. Macrophages play a crucial role in containing the infection, while T cells and cytokines contribute to the formation of granulomas. The balance between bacterial replication and immune containment determines whether the infection remains latent or progresses to active disease. Understanding these immune mechanisms is essential for developing effective vaccines and therapies.
Granulomas are a hallmark of TB and represent the host's attempt to contain the infection. They consist of a core of infected macrophages surrounded by a layer of immune cells, including T cells and fibroblasts. Granulomas can either maintain latency or break down, leading to active TB and bacterial dissemination. The stability of granulomas is influenced by various factors, including immune status and genetic predisposition.
Several factors influence the pathophysiology of TB, including the virulence of the Mycobacterium tuberculosis strain, the host's immune status, and genetic predisposition. HIV co-infection is a significant factor that increases the risk of progressing from latent to active TB. Environmental factors, such as overcrowding and malnutrition, also play a critical role in the spread and severity of TB.
Diagnosing TB involves a combination of clinical evaluation, radiographic imaging, and laboratory tests. The tuberculin skin test (TST) and interferon-gamma release assays (IGRAs) are used to detect latent TB infection, while sputum smear microscopy, culture, and molecular tests are used to diagnose active TB. Early and accurate diagnosis is crucial for effective treatment and control of TB.
The treatment of TB involves a combination of antibiotics administered over several months. The standard regimen includes isoniazid, rifampicin, ethambutol, and pyrazinamide. Directly observed therapy (DOT) is recommended to ensure adherence and prevent the development of drug-resistant TB. In addition to pharmacological treatment, addressing social determinants of health, such as housing and nutrition, is essential for successful TB management.
Preventing and controlling TB requires a multi-faceted approach, including vaccination with the Bacillus Calmette-Guérin (BCG) vaccine, early detection and treatment of active cases, and addressing social determinants of health such as overcrowding and malnutrition. Public health strategies should focus on improving living conditions and increasing access to healthcare services.
Understanding the difference between latent and active TB is crucial. Latent TB occurs when the bacteria remain dormant in the body without causing symptoms, while active TB manifests with symptoms and can spread to others. Treating latent TB helps prevent the progression to active TB. Strategies to manage latent TB include regular monitoring and preventive treatment for high-risk individuals.
Tuberculosis remains a major global health issue, particularly in low- and middle-income countries. Efforts to combat TB include improving access to diagnostics, treatment, and preventive measures, as well as addressing socio-economic factors that contribute to its spread. Global health initiatives, such as the WHO's End TB Strategy, aim to reduce TB incidence and mortality through coordinated efforts.
Ongoing research aims to develop more effective TB vaccines, shorter treatment regimens, and novel diagnostic tools. Advancements in understanding the molecular mechanisms of TB pathogenesis will contribute to the development of targeted therapies and improved public health strategies. Collaborative efforts between researchers, healthcare providers, and policymakers are essential to achieving these goals.
Understanding the pathophysiology of tuberculosis is essential for developing effective strategies to combat this infectious disease. By exploring the mechanisms involved in TB infection, immune response, and granuloma formation, we can better appreciate the complexities of TB and work towards improved treatments and preventive measures. Continued research and global efforts are crucial in the fight against tuberculosis. The integration of scientific advancements with public health initiatives will pave the way for a TB-free world.
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also impact other parts of the body, including the kidneys, spine, and brain. TB is transmitted through airborne droplets when an infected person coughs or sneezes. Despite significant advancements in medicine, TB remains a leading cause of death worldwide, particularly in low- and middle-income countries.
The pathogenesis of tuberculosis involves several stages, including initial infection, latent TB, and active TB. During initial infection, the bacterium enters the lungs and is engulfed by alveolar macrophages. However, Mycobacterium tuberculosis can evade the immune response, leading to the formation of granulomas, which contain the infection but do not eliminate it. This complex process involves multiple factors, including bacterial virulence and host immune responses.
Granulomas are a hallmark of TB and represent the host's attempt to contain the infection. They consist of a core of infected macrophages surrounded by a layer of immune cells, including T cells and fibroblasts. Granulomas can either maintain latency or break down, leading to active TB and bacterial dissemination. The stability of granulomas is influenced by various factors, including immune status and genetic predisposition.
Need Personalized Health Guidance?
Get expert advice tailored to your specific health needs from our qualified healthcare professionals.